Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers
FREEAbstract
Background:
Observational evidence suggests that mask wearing mitigates transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). It is uncertain if this observed association arises through protection of uninfected wearers (protective effect), via reduced transmission from infected mask wearers (source control), or both.
Objective:
To assess whether recommending surgical mask use outside the home reduces wearers' risk for SARS-CoV-2 infection in a setting where masks were uncommon and not among recommended public health measures.
Design:
Randomized controlled trial (DANMASK-19 [Danish Study to Assess Face Masks for the Protection Against COVID-19 Infection]). (ClinicalTrials.gov: NCT04337541)
Setting:
Denmark, April and May 2020.
Participants:
Adults spending more than 3 hours per day outside the home without occupational mask use.
Intervention:
Encouragement to follow social distancing measures for coronavirus disease 2019, plus either no mask recommendation or a recommendation to wear a mask when outside the home among other persons together with a supply of 50 surgical masks and instructions for proper use.
Measurements:
The primary outcome was SARS-CoV-2 infection in the mask wearer at 1 month by antibody testing, polymerase chain reaction (PCR), or hospital diagnosis. The secondary outcome was PCR positivity for other respiratory viruses.
Results:
A total of 3030 participants were randomly assigned to the recommendation to wear masks, and 2994 were assigned to control; 4862 completed the study. Infection with SARS-CoV-2 occurred in 42 participants recommended masks (1.8%) and 53 control participants (2.1%). The between-group difference was −0.3 percentage point (95% CI, −1.2 to 0.4 percentage point; P = 0.38) (odds ratio, 0.82 [CI, 0.54 to 1.23]; P = 0.33). Multiple imputation accounting for loss to follow-up yielded similar results. Although the difference observed was not statistically significant, the 95% CIs are compatible with a 46% reduction to a 23% increase in infection.
Limitation:
Inconclusive results, missing data, variable adherence, patient-reported findings on home tests, no blinding, and no assessment of whether masks could decrease disease transmission from mask wearers to others.
Conclusion:
The recommendation to wear surgical masks to supplement other public health measures did not reduce the SARS-CoV-2 infection rate among wearers by more than 50% in a community with modest infection rates, some degree of social distancing, and uncommon general mask use. The data were compatible with lesser degrees of self-protection.
Primary Funding Source:
The Salling Foundations.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the cause of coronavirus disease 2019 (COVID-19), has infected more than 54 million persons (1, 2). Measures to impede transmission in health care and community settings are essential (3). The virus is transmitted person-to-person, primarily through the mouth, nose, or eyes via respiratory droplets, aerosols, or fomites (4, 5). It can survive on surfaces for up to 72 hours (6), and touching a contaminated surface followed by face touching is another possible route of transmission (7). Face masks are a plausible means to reduce transmission of respiratory viruses by minimizing the risk that respiratory droplets will reach wearers' nasal or oral mucosa. Face masks are also hypothesized to reduce face touching (8, 9), but frequent face and mask touching has been reported among health care personnel (10). Observational evidence supports the efficacy of face masks in health care settings (11, 12) and as source control in patients infected with SARS-CoV-2 or other coronaviruses (13).
An increasing number of localities recommend masks in community settings on the basis of this observational evidence, but recommendations vary and controversy exists (14). The World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention (15) strongly recommend that persons with symptoms or known infection wear masks to prevent transmission of SARS-CoV-2 to others (source control) (16). However, WHO acknowledges that we lack evidence that wearing a mask protects healthy persons from SARS-CoV-2 (prevention) (17). A systematic review of observational studies reported that mask use reduced risk for SARS, Middle East respiratory syndrome, and COVID-19 by 66% overall, 70% in health care workers, and 44% in the community (12). However, surgical and cloth masks were grouped in preventive studies, and none of the 3 included non–health care studies related directly to COVID-19. Another systematic review (18) and American College of Physicians recommendations (19) concluded that evidence on mask effectiveness for respiratory infection prevention is stronger in health care than community settings.
Observational evidence suggests that mask wearing mitigates SARS-CoV-2 transmission, but whether this observed association arises because masks protect uninfected wearers (protective effect) or because transmission is reduced from infected mask wearers (source control) is uncertain. Here, we report a randomized controlled trial (20) that assessed whether a recommendation to wear a surgical mask when outside the home among others reduced wearers' risk for SARS-CoV-2 infection in a setting where public health measures were in effect but community mask wearing was uncommon and not recommended.
Methods
Trial Design and Oversight
DANMASK-19 (Danish Study to Assess Face Masks for the Protection Against COVID-19 Infection) was an investigator-initiated, nationwide, unblinded, randomized controlled trial (ClinicalTrials.gov: NCT04337541). The trial protocol was registered with the Danish Data Protection Agency (P-2020-311) (Part 10 of the Supplement) and published (21). The researchers presented the protocol to the independent regional scientific ethics committee of the Capital Region of Denmark, which did not require ethics approval (H-20023709) in accordance with Danish legislation (Parts 11 and 12 of the Supplement). The trial was done in accordance with the principles of the Declaration of Helsinki.
Participants and Study Period
During the study period (3 April to 2 June 2020), Danish authorities did not recommend use of masks in the community and mask use was uncommon (<5%) outside hospitals (22). Recommended public health measures included quarantining persons with SARS-CoV-2 infection, social distancing (including in shops and public transportation, which remained open), limiting the number of persons seen, frequent hand hygiene and cleaning, and limiting visitors to hospitals and nursing homes (23, 24). Cafés and restaurants were closed during the study until 18 May 2020.
Eligible persons were community-dwelling adults aged 18 years or older without current or prior symptoms or diagnosis of COVID-19 who reported being outside the home among others for at least 3 hours per day and who did not wear masks during their daily work. Recruitment involved media advertisements and contacting private companies and public organizations. Interested citizens had internet access to detailed study information and to research staff for questions (Part 3 of the Supplement). At baseline, participants completed a demographic survey and provided consent for researchers to access their national registry data (Parts 4 and 5 of the Supplement). Recruitment occurred from 3 through 24 April 2020. Half of participants were randomly assigned to a group on 12 April and half on 24 April.
Intervention
Participants were enrolled and data registered using Research Electronic Data Capture (REDCap) software (25). Eligible participants were randomly assigned 1:1 to the mask or control group using a computer algorithm and were stratified by the 5 regions of Denmark (Supplement Table 1). Participants were notified of allocation by e-mail, and study packages were sent by courier (Part 7 of the Supplement). Participants in the mask group were instructed to wear a mask when outside the home during the next month. They received 50 three-layer, disposable, surgical face masks with ear loops (TYPE II EN 14683 [Abena]; filtration rate, 98%; made in China). Participants in both groups received materials and instructions for antibody testing on receipt and at 1 month. They also received materials and instructions for collecting an oropharyngeal/nasal swab sample for polymerase chain reaction (PCR) testing at 1 month and whenever symptoms compatible with COVID-19 occurred during follow-up. If symptomatic, participants were strongly encouraged to seek medical care. They registered symptoms and results of the antibody test in the online REDCap system. Participants returned the test material by prepaid express courier.
Written instructions and instructional videos guided antibody testing, oropharyngeal/nasal swabbing, and proper use of masks (Part 8 of the Supplement), and a help line was available to participants. In accordance with WHO recommendations for health care settings at that time, participants were instructed to change the mask if outside the home for more than 8 hours. At baseline and in weekly follow-up e-mails, participants in both groups were encouraged to follow current COVID-19 recommendations from the Danish authorities.
Antibody and Viral PCR Testing
Participants tested for SARS-CoV-2 IgM and IgG antibodies in whole blood using a point-of-care test (Lateral Flow test [Zhuhai Livzon Diagnostics]) according to the manufacturer's recommendations and as previously described (26). After puncturing a fingertip with a lancet, they withdrew blood into a capillary tube and placed 1 drop of blood followed by 2 drops of saline in the test chamber in each of the 2 test plates (IgM and IgG). Participants reported IgM and IgG results separately as “1 line present” (negative), “2 lines present” (positive), or “I am not sure, or I could not perform the test” (treated as a negative result). Participants were categorized as seropositive if they had developed IgM, IgG, or both. The manufacturer reported that sensitivity was 90.2% and specificity 99.2%. A previously reported internal validation using 651 samples from blood donors before November 2019 and 155 patients with PCR-confirmed SARS-CoV-2 infection estimated a sensitivity of 82.5% (95% CI, 75.3% to 88.4%) and specificity of 99.5% (CI, 98.7% to 99.9%) (26). We (27) and others (28) have reported that oropharyngeal/nasal swab sampling for SARS-CoV-2 by participants, as opposed to health care workers, is clinically useful. Descriptions of RNA extraction, primer and probe used, reverse transcription, preamplification, and microfluidic quantitative PCR are detailed in Part 6 of the Supplement.
Data Collection
Participants received 4 follow-up surveys (Parts 4 and 5 of the Supplement) by e-mail to collect information on antibody test results, adherence to recommendations on time spent outside the home among others, development of symptoms, COVID-19 diagnosis based on PCR testing done in public hospitals, and known COVID-19 exposures.
Outcomes
The primary outcome was SARS-CoV-2 infection, defined as a positive result on an oropharyngeal/nasal swab test for SARS-CoV-2, development of a positive SARS-CoV-2 antibody test result (IgM or IgG) during the study period, or a hospital-based diagnosis of SARS-CoV-2 infection or COVID-19. Secondary end points included PCR evidence of infection with other respiratory viruses (Supplement Table 2).
Sample Size Calculations
The sample size was determined to provide adequate power for assessment of the combined composite primary outcome in the intention-to-treat analysis. Authorities estimated an incidence of SARS-CoV-2 infection of at least 2% during the study period. Assuming that wearing a face mask halves risk for infection, we estimated that a sample of 4636 participants would provide the trial with 80% power at a significance level of 5% (2-sided α level). Anticipating 20% loss to follow-up in this community-based study, we aimed to assign at least 6000 participants.
Statistical Analysis
Participants with a positive result on an antibody test at baseline were excluded from the analyses. We calculated CIs of proportions assuming binomial distribution (Clopper–Pearson).
The primary composite outcome (intention-to-treat) was compared between groups using the χ2 test. Odds ratios and confidence limits were calculated using logistic regression. We did a per protocol analysis that included only participants reporting complete or predominant use of face masks as instructed. A conservative sensitivity analysis assumed that participants with a positive result on an antibody test at the end of the study who had not provided antibody test results at study entrance had had a positive result at entrance. To further examine the uncertainty of loss to follow-up, we did (post hoc) 200 imputations using the R package smcfcs, version 1.4.1 (29), to impute missing values of outcome. We included sex, age, type of work, time out of home, and outcome in this calculation.
Prespecified subgroups were compared by logistic regression analysis. In a post hoc analysis, we explored whether there was a subgroup defined by a constellation of participant characteristics for which a recommendation to wear masks seemed to be effective. We included sex, age, type of work, time out of home, and outcome in this calculation.
Two-sided P values less than 0.05 were considered statistically significant. Analyses were done using R, version 3.6.1 (R Foundation).
Role of the Funding Source
An unrestricted grant from the Salling Foundations supported the study, and the BESTSELLER Foundation donated the Livzon tests. The funders did not influence study design, conduct, or reporting.
Results
Participants
A total of 17 258 Danish citizens responded to recruitment, and 6024 completed the baseline survey and fulfilled eligibility criteria. The first participants (group 1; n = 2995) were randomly assigned on 12 April 2020 and were followed from 14 to 16 April through 15 May 2020. Remaining participants (group 2; n = 3029) were randomly assigned on 24 April 2020 and were followed from 2 to 4 May through 2 June 2020. A total of 3030 participants were randomly assigned to the recommendation to wear face masks, and 2994 were assigned not to wear face masks (Figure); 4862 participants (80.7%) completed the study. Table 1 shows baseline characteristics, which were well balanced between groups. Participants reported having spent a median of 4.5 hours per day outside the home.
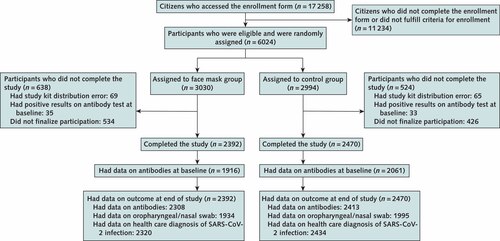
Inclusion and exclusion criteria are described in the Methods section, and criteria for completion of the study are given in the Supplement. SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2.
Table 1. Characteristics of Participants Completing the Study
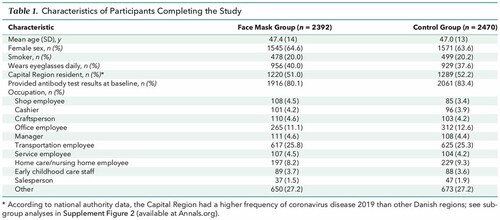 |
Adherence
Based on the lowest adherence reported in the mask group during follow-up, 46% of participants wore the mask as recommended, 47% predominantly as recommended, and 7% not as recommended.
Primary Outcome
The primary outcome occurred in 42 participants (1.8%) in the mask group and 53 (2.1%) in the control group. In an intention-to-treat analysis, the between-group difference was −0.3 percentage point (CI, −1.2 to 0.4 percentage point; P = 0.38) (odds ratio [OR], 0.82 [CI, 0.54 to 1.23]; P = 0.33) in favor of the mask group (Supplement Figure 1). When this analysis was repeated with multiple imputation for missing data due to loss to follow-up, it yielded similar results (OR, 0.81 [CI, 0.53 to 1.23]; P = 0.32). Table 2 provides data on the components of the primary end point, which were similar between groups.
Table 2. Distribution of the Components of the Composite Primary Outcome
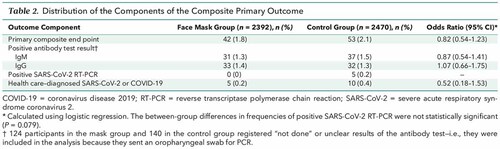 |
In a per protocol analysis that excluded participants in the mask group who reported nonadherence (7%), SARS-CoV-2 infection occurred in 40 participants (1.8%) in the mask group and 53 (2.1%) in the control group (between-group difference, −0.4 percentage point [CI, −1.2 to 0.5 percentage point]; P = 0.40) (OR, 0.84 [CI, 0.55 to 1.26]; P = 0.40). Supplement Figure 2 provides results of the prespecified subgroup analyses of the primary composite end point. No statistically significant interactions were identified.
In the preplanned sensitivity analysis, those who had a positive result on an antibody test at 1 month but had not provided antibody results at baseline were considered to have had positive results at baseline (n = 18)—that is, they were excluded from the analysis. In this analysis, the primary outcome occurred in 33 participants (1.4%) in the face mask group and 44 (1.8%) in the control group (between-group difference, −0.4 percentage point [CI, −1.1 to 0.4 percentage point]; P = 0.22) (OR, 0.77 [CI, 0.49 to 1.22]; P = 0.26).
Three post hoc (not preplanned) analyses were done. In the first, which included only participants reporting wearing face masks “exactly as instructed,” infection (the primary outcome) occurred in 22 participants (2.0%) in the face mask group and 53 (2.1%) in the control group (between-group difference, −0.2 percentage point [CI, −1.3 to 0.9 percentage point]; P = 0.82) (OR, 0.93 [CI, 0.56 to 1.54]; P = 0.78). The second post hoc analysis excluded participants who did not provide antibody test results at baseline; infection occurred in 33 participants (1.7%) in the face mask group and 44 (2.1%) in the control group (between-group difference, −0.4 percentage point [CI, −1.4 to 0.4 percentage point]; P = 0.33) (OR, 0.80 [CI, 0.51 to 1.27]; P = 0.35). In the third post hoc analysis, which investigated constellations of patient characteristics, we did not find a subgroup where face masks were effective at conventional levels of statistical significance (data not shown).
A total of 52 participants in the mask group and 39 control participants reported COVID-19 in their household. Of these, 2 participants in the face mask group and 1 in the control group developed SARS-CoV-2 infection, suggesting that the source of most observed infections was outside the home. Reported symptoms did not differ between groups during the study period (Supplement Table 3).
Secondary Outcomes
In the mask group, 9 participants (0.5%) were positive for 1 or more of the 11 respiratory viruses other than SARS-CoV-2, compared with 11 participants (0.6%) in the control group (between-group difference, −0.1 percentage point [CI, −0.6 to 0.4 percentage point]; P = 0.87) (OR, 0.84 [CI, 0.35 to 2.04]; P = 0.71). Positivity for any virus, including SARS-CoV-2, occurred in 9 mask participants (0.5%) versus 16 control participants (0.8%) (between-group difference, −0.3 percentage point [CI, −0.9 to 0.2 percentage point]; P = 0.26) (OR, 0.58 [CI, 0.25 to 1.31]; P = 0.19).
Discussion
In this community-based, randomized controlled trial conducted in a setting where mask wearing was uncommon and was not among other recommended public health measures related to COVID-19, a recommendation to wear a surgical mask when outside the home among others did not reduce, at conventional levels of statistical significance, incident SARS-CoV-2 infection compared with no mask recommendation. We designed the study to detect a reduction in infection rate from 2% to 1%. Although no statistically significant difference in SARS-CoV-2 incidence was observed, the 95% CIs are compatible with a possible 46% reduction to 23% increase in infection among mask wearers. These findings do offer evidence about the degree of protection mask wearers can anticipate in a setting where others are not wearing masks and where other public health measures, including social distancing, are in effect. The findings, however, should not be used to conclude that a recommendation for everyone to wear masks in the community would not be effective in reducing SARS-CoV-2 infections, because the trial did not test the role of masks in source control of SARS-CoV-2 infection. During the study period, authorities did not recommend face mask use outside hospital settings and mask use was rare in community settings (22). This means that study participants' exposure was overwhelmingly to persons not wearing masks.
The observed infection rate was similar to that reported in other large Danish studies during the study period (26, 30). Of note, the observed incidence of SARS-CoV-2 infection was higher than we had estimated when planning a sample size that would ensure more than 80% power to detect a 50% decrease in infection. The intervention lasted only 1 month and was carried out during a period when Danish authorities recommended quarantine of diagnosed patients, physical distancing, and hand hygiene as general protective means against SARS-CoV-2 transmission (23). Cafés and restaurants were closed through 18 May, but follow-up of the second randomized group continued through 2 June.
The first randomized group was followed while the Danish society was under lockdown. Reopening occurred (18 May 2020) during follow-up of the second group of participants, but it was not reflected in the outcome because infection rates were similar between groups (Supplement Figure 2). The relative infection rate between mask wearers and those not wearing masks would most likely be affected by changes in applied protective means or in the virulence of SARS-CoV-2, whereas the rate difference between the 2 groups would probably not be affected solely by a higher—or lower—number of infected citizens.
Although we saw no statistically significant difference in presence of other respiratory viruses, the study was not sufficiently powered to draw definite conclusions about the protective effect of masks for other viral infections. Likewise, the study had limited power for any of the subgroup analyses.
The primary outcome was mainly defined by antibodies against SARS-CoV-2. This definition was chosen because the viral load of infected patients may be only transiently detectable (31, 32) and because approximately half of persons infected with SARS-CoV-2 are asymptomatic (26, 33). Masks have been hypothesized to reduce inoculum size (34) and could increase the likelihood that infected mask users are asymptomatic, but this hypothesis has been challenged (35). For these reasons, we did not rely solely on identification of SARS-CoV-2 in oropharyngeal/nasal swab samples. As mentioned in the Methods section, an internal validation study estimated that the point-of-care test has 82.5% sensitivity and 99.5% specificity (26).
The observed rate of incident SARS-CoV-2 infection was similar to what was estimated during trial design. These rates were based on thorough screening of all participants using antibody measurements combined with PCR, whereas the observed official infection rates relied solely on PCR test–based estimates during the period. In addition, authorities tested only a small subset of primarily symptomatic citizens of the entire population, yielding low incidence rates. On this basis, the infection rates we report here are not comparable with the official SARS-CoV-2 infection rates in the Danish population. The eligibility requirement of at least 3 hours of exposure to other persons outside the home would add to this difference. Between 6 April and 9 May 2020, we found a similar seroprevalence of SARS-CoV-2 of 1.9% (CI, 0.8% to 2.3%) in Danish blood donors using the Livzon point-of-care test and assessed by laboratory technicians (36). Testing at the end of follow-up, however, may not have captured any infections contracted during the last part of the study period, but this would have been true in both the mask and control groups and was not expected to influence the overall findings.
The face masks provided to participants were high-quality surgical masks with a filtration rate of 98% (37). A published meta-analysis found no statistically significant difference in preventing influenza in health care workers between respirators (N95 [American standard] or FFP2 [European standard]) and surgical face masks (38). Adherence to mask use may be higher than observed in this study in settings where mask use is common. Some mask group participants (14%) reported adverse reactions from other citizens (Supplement Table 4). Although adherence may influence the protective effect of masks, sensitivity analyses had similar results across reported adherence.
How SARS-CoV-2 is transmitted—via respiratory droplets, aerosols, or (to a lesser extent) fomites—is not firmly established. Droplets are larger and rapidly fall to the ground, whereas aerosols are smaller (≤5 μm) and may evaporate and remain in the air for hours (39). Transmission of SARS-CoV-2 may take place through multiple routes. It has been argued that for the primary route of SARS-CoV-2 spread—that is, via droplets—face masks would be considered effective, whereas masks would not be effective against spread via aerosols, which might penetrate or circumnavigate a face mask (37, 39). Thus, spread of SARS-CoV-2 via aerosols would at least partially explain the present findings. Lack of eye protection may also have been of importance, and use of face shields also covering the eyes (rather than face masks only) has been advocated to halt the conjunctival route of transmission (40, 41). We observed no statistically significant interaction between wearers and nonwearers of eyeglasses (Supplement Figure 2). Recent reports indicate that transmission of SARS-CoV-2 via fomites is unusual (42), but masks may alter behavior and potentially affect fomite transmission.
The present findings are compatible with the findings of a review of randomized controlled trials of the efficacy of face masks for prevention (as personal protective equipment) against influenza virus (18). A recent meta-analysis that suggested a protective effect of face masks in the non–health care setting was based on 3 observational studies that included a total of 725 participants and focused on transmission of SARS-CoV-1 rather than SARS-CoV-2 (12). Of 725 participants, 138 (19%) were infected, so the transmission rate seems to be higher than for SARS-CoV-2. Further, these studies focused on prevention of infection in healthy mask wearers from patients with a known, diagnosed infection rather than prevention of transmission from persons in their surroundings in general. In addition, identified comparators (control participants) not wearing masks may also have missed other protective means. Recent observational studies that indicate a protective association between mandated mask use in the community and SARS-CoV-2 transmission are limited by study design and simultaneous introduction of other public health interventions (14, 43).
Several challenges regarding wearing disposable face masks in the community exist. These include practical aspects, such as potential incorrect wearing, reduced adherence, reduced durability of the mask depending on type of mask and occupation, and weather. Such circumstances may necessitate the use of multiple face masks during the day. In our study, participants used a mean of 1.7 masks per weekday and 1.3 per weekend day (Supplement Table 4). Wearing a face mask may be physically unpleasant, and psychological barriers and other side effects have been described (44). “Face mask policing” between citizens might reinforce use of masks but may be challenging. In addition, the wearer of a face mask may change to a less cautious behavior because of a false sense of security, as pointed out by WHO (17); accordingly, our face mask group seemed less worried (Supplement Table 4), which may explain their increased willingness to wear face masks in the future (Supplement Table 5). These challenges, including costs and availability, may reduce the efficacy of face masks to prevent SARS-CoV-2 infection.
The potential benefits of a community-wide recommendation to wear masks include combined prevention and source control for symptomatic and asymptomatic persons, improved attention, and reduced potential stigmatization of persons wearing masks to prevent infection of others (17). Although masks may also have served as source control in SARS-CoV-2–infected participants, the study was not designed to determine the effectiveness of source control.
The most important limitation is that the findings are inconclusive, with CIs compatible with a 46% decrease to a 23% increase in infection. Other limitations include the following. Participants may have been more cautious and focused on hygiene than the general population; however, the observed infection rate was similar to findings of other studies in Denmark (26, 30). Loss to follow-up was 19%, but results of multiple imputation accounting for missing data were similar to the main results. In addition, we relied on patient-reported findings on home antibody tests, and blinding to the intervention was not possible. Finally, a randomized controlled trial provides high-level evidence for treatment effects but can be prone to reduced external validity.
Our results suggest that the recommendation to wear a surgical mask when outside the home among others did not reduce, at conventional levels of statistical significance, the incidence of SARS-CoV-2 infection in mask wearers in a setting where social distancing and other public health measures were in effect, mask recommendations were not among those measures, and community use of masks was uncommon. Yet, the findings were inconclusive and cannot definitively exclude a 46% reduction to a 23% increase in infection of mask wearers in such a setting. It is important to emphasize that this trial did not address the effects of masks as source control or as protection in settings where social distancing and other public health measures are not in effect.
Reduction in release of virus from infected persons into the environment may be the mechanism for mitigation of transmission in communities where mask use is common or mandated, as noted in observational studies. Thus, these findings do not provide data on the effectiveness of widespread mask wearing in the community in reducing SARS-CoV-2 infections. They do, however, offer evidence about the degree of protection mask wearers can anticipate in a setting where others are not wearing masks and where other public health measures, including social distancing, are in effect. The findings also suggest that persons should not abandon other COVID-19 safety measures regardless of the use of masks. While we await additional data to inform mask recommendations, communities must balance the seriousness of COVID-19, uncertainty about the degree of source control and protective effect, and the absence of data suggesting serious adverse effects of masks (45).



Infection rate mored than order of magnitude too high
When the study was conducted in 30 day period in Denmark about 4,300 people got infected which is about 0.07% of population but the study registerd about 2% infection rate in the 30 day period. The discrepancy by factor of 28 is way too high. Denmark could not have 28 higher infection prevalence than the offcial rate. The multiplier of 28x would imply that by the end of 2020 all adults in Denmark would be infected.
Since the majority of infections in the study were determined by the self-administered antibody tests one must conclude that there was much higher rate of false positives than what the manufacturer of tests claimed.
For this reason the study has a fatal flaw and its conclusiosn should be dismissed. The study does not have anything interesting or valid to tell us about the efficacy of masks.
Authors' Response to Moran, Spinelli, Gains, Llor, Rand.
We thank readers for the many interesting comments and address some of them here. We agree with Brendan Moran, that the “lag” relating to infection late during the trial and time to seroconversion was to some extent captured by PCR tests. In our sample size calculation, we applied a power of 80% with an assumed infection rate of 2% in the control group. The power was ensured as the infection rate was 2.1% in the control group, and the number of participants who finalized the study was as little higher as compared to the number needed to include according to the sample size calculation. We agree with the interesting point made by Matthew A. Spinelli, David V. Glidden, Efstathios D. Gennatas, George W. Rutherford and Monica Gandhi that cluster randomization might be a good alternative to our randomization approach. However, in practical terms it might be difficult to perform such cluster randomization; will all – or just most – citizens in the towns randomized to wear masks accept to do so? – will all – or just most – citizens in the town randomized not the wear a mask accept to do so? – there are several ethical concerns. Furthermore, as SARS-CoV-2 spreads in clusters, and the number of randomized clusters should therefore be very large to ensure a nonbiased result – making such a study logistically difficult to implement. We instructed the participants in correct use of the masks, we provided high quality masks, delivered at home, free of charge and we assessed compliance through the email surveys 4 times during the study, and the worst reported compliance was accounted for in analyses. Our take is that compliance was very high – and most likely higher than what is seen during every-day use of face masks.
Hans Gaines may be right that participants might have been infected at home from asymptomatic, i.e. un-diagnosed members of their household. The participants were only asked to wear masks when outside the home consistent with public health recommendations on use of masks -- as it is hard to imagine a recommendation to wear masks at home. We also agree with Carl Llor that the circumstances have changed since April-May when we conducted our study. We do not believe that the cultural and social behavior in Denmark is so different from other countries, but we agree that habits like kissing and hugging relatives, neighbors and friends are different in different cultures – and such habits might represent a risk for SARS-CoV-2 transmission. We agree that the question of the effectiveness of masks in crowded places and when in proximity to others is important – and was not addressed in our study. We tested the effect of adding the masks to the general recommendations including the recommendation to keep a social distance of 1-2 meters - even in crowded places. However, we agree – we need more studies to assess the efficacy of masking in different settings. We would like to highlight in response the comment by Janet Rand that our study demonstrated that “the recommendation to wear surgical masks to supplement other public health measures did not reduce the SARS-CoV-2 infection rate among wearers by more than 50% in a community with modest infection rates, some degree of social distancing, and uncommon general mask use” and that “the findings, however, should not be used to conclude that a recommendation for everyone to wear masks in the community would not be effective in reducing SARS-CoV-2 infections, because the trial did not test the role of masks in source control of SARS-CoV-2 infection.” Despite these statements in our paper, some have misinterpreted our results and unfortunately, made conclusions to questions that were not addressed by our study.
To mask or not – diagnostics matter.
Bundgaard et al. present data from a randomized controlled trial (DANMASK-19) to assess whether face mask use outside home reduces risk for SARS-CoV-2 infection (1). Infection was assessed by antibody testing, PCR testing, and healthcare diagnosis. Infection occurred in 42 participants recommended mask wearing (1.8%), and 53 control participants (2.1%). 75/95 (79%) infections were diagnosed by seroconversion. Participants tested themselves for antibodies at baseline and end of intervention using a lateral flow assay.
Antibodies to SARS-CoV-2 develop in symptomatic individuals in the second week after symptom onset and occur later in less severe infections (2, 3). The incubation period is 4-6 days (4). The purpose of mask intervention is to limit exposure to SARS-CoV-2. Yet, seroconversions in the two first weeks of the intervention period may be attributed to SARS-CoV-2 exposures before intervention. The study was conducted in a period of lockdown in Denmark. In the week preceding the first intervention period, 1504 SARS-CoV-2+ cases were identified in 13,940 PCR tests (positive rate: 10.8%); in the last week of the second intervention period 306 cases were identified in 67,773 PCR tests (positive rate: 0.5%). Therefore, a burn-in intervention period before baseline serological testing would have been appropriate.
Seroconversion occurred in 1.5% (75/4862) of participants. Seroconversions were rare and warranted confirmation by secondary testing. The authors validated the test used and found a specificity of 99.5% (CI: 98.7-99.9). This validation was done by skilled laboratory personnel using plasma samples laboratory personnel (5). In DANMASK-19, testing was done by the participants themselves using whole blood specimens. If test specificity is the same under these conditions is doubtful.
Twenty incident SARS-CoV-2 infections were diagnosed by PCR testing in a healthcare setting (n=15) or at the end of the intervention (n=5). PCR tests are specific and often use multiple SARS-CoV-2 targets (1; Part 6 of the Supplement) simulating confirmatory testing. Lag time between infectious exposure and positive PCR is only 4-5 days, which reduces need for a burn-in period. There were 5 cases in the intervention group and 15 cases in the control group diagnosed by PCR (OR: 0.34; 95%CI: 0.10-0.99). If analysis is restricted to securely ascertained infections, the effect of face masks was both clinically and statistically significant. In the prespecified analysis reported in the study, this effect may be obscured by virus exposures occurring before intervention and inappropriateness of the serological diagnostic strategy applied.
Diagnostics matter also in randomized clinical trials.
References
Universal mask mandates are not supported by the evidence
The COVID-19 pandemic has led to near-universal adoption of non-pharmaceutical intervention policies in the United States, including masking in public places. Recently, Bundgaard et al [1] reported they did not find a significant protective effect of wearing surgical face masks in their randomized control trial (RCT). This result is consistent with our review of Chu et al’s meta-analysis [2] reviewing the ability of masking to reduce coronavirus transmission, in which the included studies were mostly limited by their quasi-experimental study designs and narrow healthcare-based settings.
E-values can be used to quantify the extent to which unmeasured confounding can nullify the observed results.[3] We calculated E-values for the outcomes in Bundgaard et al’s study, finding an E-value (confidence limit) of 1.74 (1) for the primary composite end point of antibodies against SARS-CoV-2 (OR=0.82, 95% CI 0.54-1.23). For presence of IgM (OR=0.87, 95% CI = 0.54-1.41) and IgG (OR=1.07, 95% CI = 0.66-1.75), the E-value (confidence limit) was 1.56 (1) and 1.34 (1) respectively. Finally, the outcome of healthcare-diagnosed SARS-CoV-2 (OR=0.52, 95% CI = 0.18-1.53) had an E-value (confidence limit) of 3.25 (1). These low E-values indicate that unobserved activities like vigilant handwashing could easily explain the findings in this study.
Although Bundgaard et al acknowledge their study’s limitations including missing data, variable adherence and absence of blinding, it is more applicable to real-world settings during the pandemic than the observational studies in Chu et al’s meta-analysis, considering Bundgaard et al used an RCT study design and focused specifically on reducing COVID-19 transmission under non-healthcare community settings. In fact, that only 7% of mask-wearers reported non-adherence appears low, considering that 100% adherence was defined as properly covering the nose and mouth and changing the mask if worn for >8 hours. In addition, participants received three-layer disposable surgical face masks, which is inconsistent with policies mandating that any cloth covering should be used. At best, the Bundgaard et al’s findings provide negative or insignificant support for public mask-wearing policies. Nonetheless, the authors should be commended for their efforts to conduct a real-world RCT on a politically charged topic.
References
Masks Work
Dear Editor,
I agree with the DANMASK-19 findings that common masks provide small protection for the wearers. But how much protection for the people around the wearers?
To get a full picture of the masks’ protective effect, an ideal trial should separate the mask group from the non-mask group. If a trial mixes two groups together, their infection rates will be distorted. In other words, the non-mask group’s infection rate will be underestimated because the non-maskers are benefitting from the mask group’s source control, while the mask group’s will be overestimated because the maskers are suffering from the non-mask group’s spreads.
A German study [1] estimates that the effects of mandating face mask use in public would reduce the growth rates of infections by 40% to 60%. This is a clear picture of the impact of a face mask mandate on infections because the mask and non-mask groups in the study didn’t affect each other.
References
To mask or not – diagnostics matter.
Bundgaard et al. present data from a randomized controlled trial (DANMASK-19) to assess whether face mask use outside home reduces risk for SARS-CoV-2 infection (1). Infection was assessed by antibody testing, PCR testing, and healthcare diagnosis. Infection occurred in 42 participants recommended mask wearing (1.8%), and 53 control participants (2.1%). 75/95 (79%) infections were diagnosed by seroconversion. Participants tested themselves for antibodies at baseline and end of intervention using a lateral flow assay.
Antibodies to SARS-CoV-2 develop in symptomatic individuals in the second week after symptom onset and occur later in less severe infections (2, 3). The incubation period is 4-6 days (4). The purpose of mask intervention is to limit exposure to SARS-CoV-2. Yet, seroconversions in the two first weeks of the intervention period may be attributed to SARS-CoV-2 exposures before intervention. The study was conducted in a period of lockdown in Denmark. In the week preceding the first intervention period, 1504 SARS-CoV-2+ cases were identified in 13,940 PCR tests (positive rate: 10.8%); in the last week of the second intervention period 306 cases were identified in 67,773 PCR tests (positive rate: 0.5%). Therefore, a burn-in intervention period before baseline serological testing would have been appropriate.
Seroconversion occurred in 1.5% (75/4862) of participants. Seroconversions were rare and warranted confirmation by secondary testing. The authors validated the test used and found a specificity of 99.5% (CI: 98.7-99.9). This validation was done by skilled laboratory personnel using plasma samples laboratory personnel (5). In DANMASK-19, testing was done by the participants themselves using whole blood specimens. If test specificity is the same under these conditions is doubtful.
Twenty incident SARS-CoV-2 infections were diagnosed by PCR testing in a healthcare setting (n=15) or at the end of the intervention (n=5). PCR tests are specific and often use multiple SARS-CoV-2 targets (1; Part 6 of the Supplement) simulating confirmatory testing. Lag time between infectious exposure and positive PCR is only 4-5 days, which reduces need for a burn-in period. There were 5 cases in the intervention group and 15 cases in the control group diagnosed by PCR (OR: 0.34; 95%CI: 0.10-0.99). If analysis is restricted to securely ascertained infections, the effect of face masks was both clinically and statistically significant. In the prespecified analysis reported in the study, this effect may be obscured by virus exposures occurring before intervention and inappropriateness of the serological diagnostic strategy applied.
Diagnostics matter also in randomized clinical trials.
References
This study design would not even proof that a 100% protection has a protective effect
Imagine a 100% perfect protection against COVID-19 (a hermetic room), what outcome should be expected for this by-definition safe group using this study design?
Here is the math only for estimating
- the false-positive antibody-tests
- positive test due to before-baseline infections
But as the study design grants protection at average only 4.5 hours/day infections outside the room should be added to the calculated expectations (in the study false-classified as noneffective protection).
The study reports antibody testing has an estimated 99,2% specificity. For about 2400 tests this leads to an expectation of 2400*0.008=19 false-positive tests in each antibody test group.
IgG-antibodies form very delayed. So in non-increasing rate of new infections (as the case in 05/2020 in Denmark) about 80% of all true-positive IgG tests at study-end show infections before study-baseline. So the expectation of positive tests due to before-baseline infections in the control group is 10.4 (80% of 13 (=32-19) „true-positive“ IgG tests)
The mentioned false-detection arises solely to from a test-property (specificity) and before-baseline events, so the expectations for the control group for false-positive test (19) and for true-positive tests due to before-baseline infections (10.4) equals the expectations for the safe group, adding up to: expectation(IgG-SafeGroup)=29.4
IgM responds from >2-6 weeks after infection. So about 50% of the IgM true positive tests are likely due to before-baseline infections. Analogue to above 19 false positive and 9 positive IgM tests (50% of 18 (=37-19) „true-positive“ IgM tests) due to before-baseline infections sum up to: expectation(IgM-SafeGroup)=29
PCR-tests hardly suffer from specifity and time lags in the study, so no positive PCR-tests should be expected in the safe group: expectation(PCR-SafeGroup)=0
A temporally evenly distributed health care diagnosis during study will again suffer from the delay from infection to diagnosis (first 9 days (=30% of 30 days) diagnosis will likely show before-baseline infections). So 0,3*10=3 cases are likely due to before-baseline infections and have to be expected for the safe group as well: expectation(HealthCare-SafeGroup)=3
Even without additional expected infections at home, friends etc. - falsely assigned as inside the hermetic room the expected outcome in the by-definition safe group is already about 75% of the control outcome (or 90% of the face-mask-group).
Altogether this study design expects for a by-definition 100%-protection:
- measure an Odd Ratio of ≥0.75 (≤25% protection),
- include OR=1 (i.e. no-protection-at-all) in the 95%-Confidence Interval and
- exclude OR≤0.4 (≥60% protection) from 95%-CI
The effectiveness of mask recommendation (mainly outdoors) is questionable, for overlooked reasons
The DANMASK-19 (1) conclude: “The recommendation to wear surgical masks to supplement other public health measures did not reduce the SARS-CoV-2 infection rate among wearers… The difference was not statistically significant, the 95% CIs are compatible with a 46% reduction to a 23% increase in infection.”
Two editorialists (2) state: “Across all analyses odds ratios were approximately 0.8, consistent with a 20% reduction in incident SARS-CoV-2 infection if masks are recommended. The sample size was insufficient to determine the statistical significance of a 20% reduction”. However, 52 participants in the mask group and 39 control participants reported COVID-19 in their household, that might be considered as randomized clusters. Assuming the same (or proportional) numbers of Covid-19 and similar households’ denominators, summing the Sars-CoV-2 infections of each group with the COVID-19 of its households, the mask group plus households experienced more infections/diseases than the control group plus households. Moreover, 40% of face mask group reduced physical activity (1).
The criticism that “the antibody-positive results in both intervention and control groups could have been false positives” (2), biasing the findings towards the null, does not apply to the reported households’ COVID-19.
The criticism that “only 46% of those in the intervention group reported adherence” (2) exactly as instructed, weakens the editorialists’ thesis indeed, because infection, the primary outcome, occurred in 2.0% of “adherents”, further approaching the control group’s 2.1%.
The editorialists point that the intervention group females had less infections (odds ratio, 0.65; 0.38-1.12 [please note: males 1.12; 0.59-2.12]), because women “may be more likely to adhere” (2). Inconsistently, their citation (3) shows that women indeed are more compliant than men with each of ten restraining measures, and significantly so in three, including handwashing and distancing, but not with wearing face masks.
The mechanistic evidence that masks reduce wearer exposure and block his/her respiratory droplets implies specularly that microorganisms eventually multiplying in the infected persons’ airways are in turn blocked at each exhalation and partially re-inhaled, increasing the cumulative viral load and the infection, and contagiousness (4). This overlooked mechanism works in the opposite direction to the protective one: only well-designed trials can establish which net effect prevails at the community level. In the Hajj pilgrims trial (5) the net effect outdoors shifted towards an excess of respiratory infections in mask wearers (and perhaps in pilgrims sharing tents with others in the mask group). Wearing masks long and everywhere is not evidence-based.
References
Disclosures:
There are no conflicts of interest to disclose.
No future trials are needed!
I respectfully disagree with Dr. Bundgaard that additional trials are needed to help answer the question of protective benefit masks in COVID-19. We had 12 RCTs (1) from influenza and other respiratory viruses that showed us there was no added benefit from mask use. Despite this compelling evidence, we believed that the situation was different with SARS-2 in the presymptomatic phase. With the DANMASK 19, powered with 6000 individuals, it is consistent with all previous trials of mask benefit that the effects are negligible. We need to show integrity in mandating masks when the evidence CLEARLY does not support such a measure. Neither has there been any additional benefit in countries that have been more adherent to masks. The only evidence based conclusions we can recommend to the public are to avoid crowds and to enhance hand hygiene. Nothing more!
1. Chou R, Dana T, Jungbauer R, et al. Masks for Prevention of Respiratory Virus Infections, Including SARS-CoV-2, in Health Care and Community Settings : A Living Rapid Review. Ann Intern Med. 2020 Oct 6;173(7):542-555. doi: 10.7326/M20-3213. Epub 2020 Jun 24. PMID: 32579379; PMCID: PMC7322812.
External validity of these results to hard-hit areas.
Dear Editor,
Bundgaard et al. showed in their randomized controlled trial [1] that face mask use supplementing other public health strategies did not significantly reduce SARS-CoV2 infection in people wearing the mask. Apart from the limitations of the study mentioned by the authors themselves, mainly the low face mask wear adherence and the lack of assessment of whether masks could decrease disease transmission from mask wearers to others, there are other variables that can make generalization of these results difficult. The randomized controlled trial design is irrefutably the best method in clinical research addressing interventions and we have to applaud the authors for conducting such a great trial in a short period of time, but this trial was conducted in a country with a low-moderate incidence of COVID-19 and during lockdown (April and May 2020).
People in many areas of the world are less likely to avoid public places and stay home than residents of Denmark. Social distancing could qualify as an oxymoron in Southern Europe, South America, the United States and citizens of many other crowded parts of the world, where walking arm-in-arm with friends, eating out in crowded restaurants and terraces, or kissing relatives, neighbors and friends are part of their cultures. There is now solid evidence that individuals in poor health are more susceptible to serious illnesses [2]. In Southern Europe, for example, low-paid employees are less likely to do their jobs from home and taking public transport to crowded workplaces might lead to more contagions, as are families pushed into housing with insufficient space.
The “real life conditions” in many areas in the world are quite different from Denmark. We should ask if this modest protection of face mask wearers from infection with SARS-Cov-2 in this country would have been the same if this trial had been conducted in crowded areas with no curfew. We agree with the authors that more well-conducted studies are needed before drawing a conclusion like this.
References
Comment on: Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers
To The Editor,
The authors are to be commended for their contributions regarding the efficacy of face masks in mitigating the risk of transmission of SARS-CoV-2 infection (1). However, these findings should be interpreted with caution due to a number of confounding variables that were not accounted for in the study design.
Firstly, the instruction guide provided on how to wear a mask were extremely brief. It was advised that participants “place the mask over the nose and under the chin” and to “remember hand hygiene when using the mask” but no guidance was offered regarding appropriate use of the mask while it was worn, nor safe disposal of the mask when it was no longer needed. Self-contamination by touching the mask with contaminated hands after it has been donned, sharing face masks with others and reusing masks is recognised as a potential risk of SARS-CoV-2 transmission (2). Detailed and explicit instructions should have therefore been given on safe and appropriate usage of medical masks.
Furthermore, it was recommended that masks should be changed every eight hours. This eight-hourly time frame was based on World Health Organisation (WHO) guidance at the time of the trial (April-May 2020) according to the authors. However, to our knowledge, WHO recommendations at this time were that a medical mask should be replaced every six hours, or when damp or soiled (2,3). Therefore it would have been prudent to issue guidance to participants on replacing a mask within this time frame or when wet, soiled or damaged, as extended use of a mask may risk contamination with the SARS-CoV-2 virus.
In addition, adherence to mask-wearing was not only poor but poorly assessed. Only 46% of participants wore the mask as recommended, as measured through a single question (“are you using the mask according to our recommendation?”) on a weekly survey. The subjective nature of such an approach lends itself to self-reporting bias due to differences between individuals in perceiving how well they followed recommendations (4). This could have been mitigated through further questioning on the survey to more objectively estimate compliance, such as enquiring about the duration and frequency of use (5).
In summary, we believe that the conclusions drawn by this study are weak due to omissions in the study design and the potential benefits of mask-wearing as protection against SARS-CoV-2 may therefore have been missed.
References
Corresponding authors:
Suliman Ahmad, Zoe Gan
Faculty of Life Sciences & Medicine, King’s College London
Conflict of interest: None to declare
Mask effect with low prevalence
Perhaps your article can be interpreted as saying that at a time with low prevalence, especially compared with the current daily rates, mask wearing confers at best minimal benefit. Here in South Dakota, other than factory transmission by a symptomatic worker, we had virtually no spread of Covid this spring and summer, I saw a few abnormal Covid chest xrays per month. Now we are at the breaking point, I see several abnormal Covid chest xrays per day.
Yet another case of trial external validity demolished by incongruous intervention features.
Dear Editor,
This trial resembles in many aspects the ‘Parachute use to prevent death and major trauma when jumping from aircraft: randomized controlled trial’ published in 2018 by Robert W Yeh. (1) Both present non-statistically significant results on major outcomes. They both fail to reject the null hypothesis that state that there is no effect in using a parachute when jumping from aircraft to prevent death or major trauma (1) and there is no effect in reducing respiratory infections when using facial masks in the community (2). In Yeh’s study, the aircraft was on the ground and in Bundgaard’s trial, people in the community do not vastly wear facial masks, only participants in the experimental group do. SARS-CoV-2 transmission may occur by mouth, nose or eye exposure. (3) Participants in the experimental group when in close contact with other people, that do not contain air droplets by using facial masks, were exposed to similar risk of eye SARS-CoV-2 infection as the control group. If the plane was on the ground, participants from the experimental group faced the same risk as the control group. Without widespread facial mask use in the community, the protective nature of facial masks (i.e. droplets containment) remains severely compromised in close encounters. Such performance bias pose serious constrains and challenges in effectiveness trial studies design and may induce error in result interpretation and decision making in health interventions. (4) The critical appraisal of the intervention features in real life settings is warranted.
1 YEH, Robert W., et al. Parachute use to prevent death and major trauma when jumping from aircraft: randomized controlled trial. bmj, 2018, 363.
3 WU, Ping, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA ophthalmology, 2020, 138.5: 575-578.
Authors' Response to comments
Authors Henning Bundgaard and Kasper Iversen’s response to Tuan Nguyen
Thanks for this interesting analysis. It should be noted that the meta-analysis was not related to SARS-CoV-2, which might be a limitation. Also, our pre-defined statistical analysis plan did not include the Bayesian approach.
Authors Henning Bundgaard and Kasper Iversen’s response to Constantine Manthous
Thank you for your comment. The study participants were not instructed to wear masks at home as this is not part of the authorities Public Health Recommendations. In the paper we accounted for reported diagnosed COVID-19 in the household, but of course – asymptomatic household members might have been missed. We consider that masking at home would not be realistic, so this potential limitation is after all just another reflection of the real-world setting of the trial.
Authors Henning Bundgaard and Kasper Iversen’s response to Hadi Ali, Gunce Kaya and Khameinei Ali
Thank you very much for these comments. We have been as open and clear in our reporting. We agree that randomized clinical trials (RCTs) may suffer from many limitations or biases, but still RCTs are the most widely used design to obtain clinical documentation. For the same reason, more than one trial is often requested before firm recommendations are made. This relates to circumventing some of the potential biases in one study and to ensure external validation. On this basis we most certainly hope that others are perming new trials to expand our knowledge and build a stronger foundation for future recommendations. In the paper we really tried our very best to be as judicious as possible in the conclusion.
Authors Henning Bundgaard and Kasper Iversen’s response to Edward Siguel
Thank you for your interesting comments. Testing a hypothesis is the backbone of science, and although a hypothesis might be considered common sense, we still need to conduct the proper studies under the right circumstances to accept or reject a hypothesis. Here the focus is source control, i.e. whether the wearer of the face mask is protected from getting infected.
Authors Henning Bundgaard and Kasper Iversen’s response Matthew A. Spinelli, David V. Glidden, Efstathios D. Gennatas, George W. Rutherford and Monica Gandhi
Thanks for these interesting comments. We agree that cluster randomization might be a good alternative to RCT’s. However, in practical terms it might be difficult to perform a face mask trial clustering; will all – or just most – citizens in the towns randomized to wear masks accept to do so? – will all – or just most – citizens in the town randomized not the wear a mask accept to do so? – there are several ethical concerns. Furthermore, as SARS-CoV-2 spreads in clusters and the number of clusters should therefore be very large to ensure a nonbiased result – making a cluster study even more difficult. We instructed the participants in correct use of the masks, we provided high quality masks, delivered at home, free of charge and we assessed compliance through the email surveys 4 times during the study, and the worst reported compliance was in the analyses. Our take is that compliance was very high – and most likely higher than what is seen during every-day use of face masks.
Authors Henning Bundgaard and Kasper Iversen’s response to Michael Cook
In our study we assessed if masks offer a protective effect to uninfected wearers - and not if masks reduced the transmission of SARS-CoV-2 from infected mask wearers out into the community.
Authors Henning Bundgaard and Kasper Iversen’s response to Simon Thompson
Thank you for these comments. Our contribution was to provide research data on efficiency of face masks. Authorities have to include all other data and other aspects as referred to into consideration when developing the guidelines for the citizens.
Authors Henning Bundgaard and Kasper Iversen’s response to Max Longin
Thank you for these comments. The participants in the mask group were recommended to wear masks when outside the home. At entry – and at end of study IgG and IgM were determined, and only participants reporting not to have or have had COVID-19 were eligible. IgG and/or IgM positive participants at baseline were excluded from the analyses. The primary outcome was a composite outcome of antibody test results, PCR and diagnosed COVID-19 in the healthcare system. COVID-19 diagnosed household members were accounted for. However, asymptomatic household members were not accounted for. The issue of before entry infection and just before end-of-study infection is true for both groups.
Authors Henning Bundgaard and Kasper Iversen’s response to Janet Rand
Thank you for your comments. Our study demonstrate that “the recommendation to wear surgical masks to supplement other public health measures did not reduce the SARS-CoV-2 infection rate among wearers by more than 50% in a community with modest infection rates, some degree of social distancing, and uncommon general mask use.” As you also mention, our study also highlight that “the findings, however, should not be used to conclude that a recommendation for everyone to wear masks in the community would not be effective in reducing SARS-CoV-2 infections, because the trial did not test the role of masks in source control of SARS-CoV-2 infection.”
Despite these statements, we cannot control how our study is being interpreted.
Authors Henning Bundgaard and Kasper Iversen’s response to Dr Rosamond A K Jones
Thank you for your comments. Our aim was to provide scientific documentation for the efficiency of face masks for the wearer. We agree that masking may have a number of side effects – including psychological side effects – also in children. However, we have not assessed the psychological aspects of wearing face masks and further studies are needed to address this.
Authors Henning Bundgaard and Kasper Iversen’s response to Brenda Marfin
Thank you for your comments. We are sorry to hear about your and your husbands’ situation. Our study finding is one part of the puzzle for understanding the effects of mask. We have been very clear that we studied the efficiency of masks protection for the wearer – not the effects of face masks when used by an infected individual (source control). We have made an effort to communicate the results in an objective manner and to emphasize the limitations of the study in order to accommodate the considerations you also raise. We cannot control how our study is being interpreted by individuals.
Authors Henning Bundgaard and Kasper Iversen’s response to Ambuj Kumar
Thank you for the comments. Our aim was to provide scientific documentation for the protective efficiency of face masks for the wearer in addition to other protective means. The efficiency was not assessed as a dichotomous outcome – except an expected lowest outcome had to be applied in the power calculation.
Authors Henning Bundgaard and Kasper Iversen’s response to Eric Thompson
Our study finding is one part of the puzzle for understanding the effects of mask. Formulation of policy recommendations should take into account all the research and knowledge available, and we leave this to the policy makers.
Authors Henning Bundgaard and Kasper Iversen’s response to El Rowan
Testing adherence to recommendations in a community-based, randomized controlled trial such as this is difficult, as the real-life setting does not allow individual control. The question of true adherence will always be a question unanswered in a community-based randomized trial where the participant is the active part in carrying out the intervention – whether it be wearing a mask, taken their medicine as recommended, doing their exercise etc. - and it will in the end always depend on the honesty and self-reflection of the participant. Like in most drug trials we rely on the fact that the volunteer participation motivates honest answers. But yes, we – and others - cannot be sure.
Authors Henning Bundgaard and Kasper Iversen’s response to Hans Gaines
Thank you for your comments. Our study investigated the “effectiveness of adding a mask recommendation to other public health measures to prevent SARS-CoV-2 infection”. We agree that participants might have been infected at home from asymptomatic members of their household. The participants were only asked to wear masks when outside the home. We consider that this reflects the generally used recommendations as it is hard to imaging a recommendation to wear masks at home.
Authors Henning Bundgaard and Kasper Iversen’s response to Eemil Zhang
Thank you for your input. The Lammers, Crusuis, Gast 2020 paper you refer to discuss that the perception of the spread – whether linear or exponentially biased – will affect the way people act on the recommendations. However, the SARS-CoV-2 infection rate was not growing exponentially in Denmark during the study period. Moreover, if the question is whether people perceive it as exponentially growth - and thus would change their behavior thereafter - this perception would be expected to be similar between the groups.
Authors Henning Bundgaard and Kasper Iversen’s response to Brendan Moran
Thanks for your comments. We agree, the “lag” relating to infection late during the trial and time to seroconversion was to some extent captured by the PCR. In our sample size calculation, we applied a power of 80% with an assumed infection rate of 2% in the control group. The power was ensured as the infection rate was 2.1% in the control group, and the number of participants who finalized the study was as little higher as compared to the number needed to include according to the sample size calculation.
Paper may suggest that masks may indeed be effective.
Did not the article report that a much larger number of mask wearing subjects had Covid 19 in their households? If so, a significantly higher rate of Covid 19 infection would have been expected given the known household transmission. Yet Covid infection despite all the other uncertainties in the protocols, was less in the masked group.
The failure of the study to have mask wearers not be “taxed” with wearing masks at home , even if there was known Covid 19 present raises scientific, public health and ethical questions. On that basis it may be due for retraction. The imprecision due to multiple uncontrolled factors similarly makes it a study, however well intentioned, that should have been rejected as it is inconclusive and does not clearly guide the path for how a useful one might be done.
Maskless driving as high risk for catching coronavirus
To Editor
In the United States, the number of daily new cases with COVID-19 keeps breaking global records. After seven months of preventive measures mandated and practiced, this wrong direction should be introspecting.
COVID-19 is caused by infection with the coronavirus SARS-CoV-2 and spreading mainly via airborne transmission so that wearing face masks is the most effective prevention measure for the public(1). However, Bundgaard et al reported a marginal and inclusive mask-based prevention from outdoor infection based on their randomized controlled trial(2). That study didn’t consider stratified outdoor time because the outdoor activity could be situational in terms of coronavirus transmission, such as gathering and driving.
Currently in the States, there is no curfew or strict lockdown. By contrast, many working places remain active at reduced density and automobiles are running all over the streets and highways day and night. Of people with face masks, approximately a half don’t wear their masks correctly in the public and most people inside their cars don’t wear masks at all.
It is safe to stay inside the car, however, can be a misperception regarding SARS-CoV-2. People usually feel safe when getting into their cars so that they take off the masks immediately once inside the cars. Automobiles are equipped with cabin air filters which are designed to keep air pollutants such as dust and pollen out of the passenger compartment. However, these filters can trap particles only as small as 0.3~0.5 microns, with a filtration efficiency of 50–90% where the filtration effectiveness decreases with decreasing particle size.(3) Therefore, these cabin filters are not designed to filter out the coronavirus whose average size is 0.1 microns (with a range of 0.06~0.14 micron) so that inside the car is not coronavirus-proof.
Inadequate and insufficient mearing of face masks(4) may partly explain the current surges in daily new cases. In the peaking times of this pandemic, when one drives a car with air ventilated from outside, the risk of airborne transmission can be increased with the speed of the vehicle. SARS-CoV-2 in aerosols (with sizes similar to the coronavirus) remains infectious for hours(5) so that 10-20 fold-accelerated exposure to the public air is a high risk but was neglected by the randomized trial.
“The goal of reliably filtering coronavirus from a vehicle cabin has myriad challenges,” as clarified and warned by the Society of Automotive Engineers International (https://www.sae.org/news/2020/03/coronavirus-cabin-air-filtration). Maskless driving can be searching for SARS-CoV-2.
Conflict of interest: None to declare.
Funding: None.
References:
Disclosures:
None to declare.
Evidence from randomized controlled trials on the surgical masks’ effect on the spread of respiratory infections in the community
Dear Editor:
In the Bundgaard et al. randomized controlled trial (RCT)1, face mask use supplementing other public health measures did not significantly reduce SARS-CoV2 infection in people wearing the mask, albeit the results cannot exclude a 46% reduction or a 23% increase in infection among mask wearers. These findings seem to confirm the notion that recommendations on the public use of respiratory devices to prevent SARS-CoV-2 infection have low certainty evidence.2
Indirect supportive data can come from studies dealing with the protection offered by surgical masks in influenza-like illness (ILI). We conducted a systematic review and meta-analysis of RCTs (PROSPERO ID: CRD42020178913) on the use of surgical masks in the community as a mean to prevent the spreading of ILI. The population included students and households’ members of any age and sex. The main outcome was the risk of ILI among mask users vs non-users. Eligible studies included RCTs published between January 1, 2005 and April 7, 2020 in English language. Two blinded reviewers independently screened the papers identified through a search strategy including umbrella and traditional reviews, based on PubMed/Medline and Embase libraries.3
Out of 422 papers, 11 RCTs assessed the role of wearing versus not wearing surgical masks on ILI prevention. Overall, the studies enrolled a total of 7469 subjects. The pooled random effect relative risk (RR) for face mask protection was 0·92 (95% CI:0·81-1·04), suggesting that wearing surgical masks in the community confer no significant protection against ILI in mask wearers. It should be noted that most studies in our meta-analysis were underpowered, and that 73% of them reported a poor adherence of participants to mask use. A sub-analysis of few high compliance studies showed a RR of 0·67, 95% CI:0·46-0·99.
Notably, the type of mask and the securing system may largely influence the filtering effectiveness of face masks, with surgical or procedural masks secured with elastic ear lobes showing the least filtration efficiency.4
At variance with observational studies, randomised trials have failed, up to now, to clearly document the utility of wearing masks to prevent SARS-CoV2 infection. A public health intervention promoting face mask use, is usually implemented at units larger than that of individuals. Hence, we suggest that a convenient study design would be a cluster randomised trial assessing, in a factorial way, the impact of promoting the combination of different components of individual protection on the prevention of SARS-CoV2 spreading.
References
Corresponding author:
Prof. Luigi Naldi
Study Center of the Italian Group for Epidemiological Research in Dermatology (GISED)
Via Clara Maffei 4, 24121 Bergamo (Italy)
Tel. +39035223753
e-mail luiginaldibg@gmail.com
Another possible source of bias
Dear Editor:
Performing a large intervention study on the population level is surely a huge effort, and the authors must be applauded for setting out to assess the effectiveness of “medical” type face masks in addition to measures of social distancing in preventing SARS-CoV-2 infection. Thereby, they followed a conclusion from a recent meta-analysis on the topic, which had found a clear indication of a protection from virus transmission by - particularly N95 or surgical quality - face masks, but noted considerable uncertainty of evidence [1].
The randomised controlled trial design chosen is undisputedly the gold standard method in clinical research addressing interventions. However, its application in a population setting instead of a relatively well-controlled, quasi experimental clinical setting is not without pitfalls, some of which have already been outlined by other scientific comments. Another particular confounding effect related to the intervention not being amenable to blinding, and also biasing the results towards “no effect”, is the possibility that participants in the intervention group may have changed their relevant behaviour once wearing masks, notwithstanding similar behaviour at baseline. Such a change would most plausibly happen in terms of respecting less the fundamental rules of social distancing, feeling protected well enough by the face mask, thereby increasing infection risk.
From a general perspective, the DANMASK-19 study results, independent from other issues likely biasing the results towards “no effect” as discussed in other comments, cannot quantify efficacy, i.e. the maximum possible effect of an intervention, but effectiveness, i.e., the intervention effect observed under “real life conditions”. Effectiveness is often (much) smaller than efficacy, owing to manifold interferences, perhaps including the confounding effect suggested above. As “real life conditions” largely mean the societal and historical context, the following conclusions can be drawn: (i) effectiveness as observed in the study cannot be easily generalised; (ii) efficacy of wearing adequate masks adequately is underestimated by the current results, to an unknown extent; (iii) contrary to clinical interventions, the (individually) randomised controlled trial cannot necessarily be regarded as gold standard to assess efficacy on the population level.
[1] Derek K Chu, Elie A Akl, Stephanie Duda, Karla Solo, Sally Yaacoub, Holger J Schünemann, COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet 2020 Jun 27;395(10242):1973-1987
Data raise concerns about mask-wearing causing potentially harmful reductions in physical activity
Dear Editor,
This randomised control study by Bundgaard et al. did not find face-mask wearing to have a significant effect on SARS-COV2 infection. However, the data indicate a concerning decrease in levels of physical activity among the mask-wearing cohort, which the article does not explore.
The results of the tertiary end points published in the supplementary material suggest that levels of physical activity decreased in 40% of the mask-wearing cohort. This potential effect of mask wearing is worthy of further study. Unfortunately, the decrease in physical activity reported in this trial cannot be compared to a control as the non-mask-wearing cohort were not asked about their level of exercise in the study period. Also, trial participants were not asked to quantify the change in their physical activity, which would indicate how much of a concern this decrease should raise.
The WHO Global Action Plan on Physical Activity 2018-2030 highlights physical inactivity as a major cost to health systems and society due to resultant ill health. If mask wearing results in reduced levels of physical exercise, and therefore worse physical health, this risk should be taken into account both by individuals and those responsible for health policy.
Additionally, results regarding levels of sick leave and bacterial infection in the two groups have yet to be published. May I ask when the authors expect this information to become available?
Evidence from randomised controlled trials on the surgical masks’ effect on the spread of respiratory infections in the community
Dear Editor:
In the Bundgaard et al. randomized controlled trial (RCT)1, face mask use supplementing other public health measures did not significantly reduce SARS-CoV2 infection in people wearing the mask, albeit the results cannot exclude a 46% reduction or a 23% increase in infection among mask wearers. These findings seem to confirm the notion that recommendations on the public use of respiratory devices to prevent SARS-CoV-2 infection have low certainty evidence.2
Indirect supportive data can come from studies dealing with the protection offered by surgical masks in influenza-like illness (ILI). We conducted a systematic review and meta-analysis of RCTs (PROSPERO ID: CRD42020178913) on the use of surgical masks in the community as a mean to prevent the spreading of ILI. The population included students and households’ members of any age and sex. The main outcome was the risk of ILI among mask users vs non-users. Eligible studies included RCTs published between January 1, 2005 and April 7, 2020 in English language. Two blinded reviewers independently screened the papers identified through a search strategy including umbrella and traditional reviews, based on PubMed/Medline and Embase libraries.3
Out of 422 papers, 11 RCTs assessed the role of wearing versus not wearing surgical masks on ILI prevention. Overall, the studies enrolled a total of 7469 subjects. The pooled random effect relative risk (RR) for face mask protection was 0·92 (95% CI:0·81-1·04), suggesting that wearing surgical masks in the community confer no significant protection against ILI in mask wearers. It should be noted that most studies in our meta-analysis were underpowered, and that 73% of them reported a poor adherence of participants to mask use. A sub-analysis of few high compliance studies showed a RR of 0·67, 95% CI:0·46-0·99.
Notably, the type of mask and the securing system may largely influence the filtering effectiveness of face masks, with surgical or procedural masks secured with elastic ear lobes showing the least filtration efficiency.4
At variance with observational studies, randomised trials have failed, up to now, to clearly document the utility of wearing masks to prevent SARS-CoV2 infection. A public health intervention promoting face mask use, is usually implemented at units larger than that of individuals. Hence, we suggest that a convenient study design would be a cluster randomised trial assessing, in a factorial way, the impact of promoting the combination of different components of individual protection on the prevention of SARS-CoV2 spreading.
References
Multiple bias towards the Null
Any study to evaluate the effectiveness of wearing masks should be done with a very careful methodological approach in order to avoid multiple sources of error. We have learned so far that the risk of SARS-CoV-2 infection through the respiratory route is very high specially at home, at lunch and coffee-break times, where nobody uses any mask protection. In this randomized open trial, there was no control over these sources of infection. Besides, only 46% of participants wore the mask as recommended, a very low adherence level. With that in mind, I would expect the results to be biased towards no association between the use of masks and the risk of SARS-CoV-2 infection as the authors stated
A Bayesian interpretation of the effect of face mask on SARS-Cov-2 infection
Dear Editor:
I would like to offer an alternative interpretation of the DANMASK-19's data [1]. My interpretation centers on the question: what is the probability that face mask wearing reduces the risk of SARS-Cov-2 infection. This question can only be answered by a Bayesian approach that updates our pre-existing knowledge with new evidence [2].
Our pre-existing knowledge is informed by a recent meta-analysis which shows that surgical face mask is associated with a 13% reduction in the risk of acute respiratory infection (risk ratio [RR], 0.87; 95% confidence interval [CI], 0.74 to 1.04) [3]. Note that the average risk reduction reported in this meta-analysis is statistically comparable with that observed in the DANMASK-19 study (i.e., 18% risk reduction; RR, 0.82; 95% CI, 0.54 to 1.23).
When the distribution of relative risks obtained from the meta-analysis [3] is updated by the DANMASK-19's relative risk [1] by the Bayesian theorem [4], the new relative risk is 0.85, with 95% credible interval ranging from 0.72 to 0.99. Moreover, the probability that face mask wearing reduces the risk of SARS-Cov-2 infection by at least 50% is zero. Nevertheless, there is a 93% chance that face mask wearing reduces the risk SARS-Cov-2 infection by at least 5%.
Thus, in settings with moderate Covid-19 infection (such as Denmark) the updated evidence suggests that wearing face mask may modestly protect the wearers from infection with SARS-Cov-2.
References:
[1] Bundgaard H, et al. Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers: A Randomized Controlled Trial. Ann Int Med 18/11/2020.
[2] Ferreira D, et al. Theory and practical use of Bayesian methods in interpreting clinical trial data: a narrative review. Br J Anaesth. 2020;125(2):201-7.
[3] Wang MX, et al. Effectiveness of Surgical Face Masks in Reducing Acute Respiratory Infections in Non-Healthcare Settings: A Systematic Review and Meta-Analysis. Front Med 2020;7:564280.
[4] R codes available here: https://github.com/tuanvnguyen/Bayesian-analysis/blob/main/Normal-Normal%20model
Masks didn't work? Not so fast
In the November 18 issue of Annals, Bundgaard et al conclude: “The recommendation to wear surgical masks to supplement other public health measures did not reduce the SARS-CoV-2 infection rate among wearers . . . (1)“ Not so quick. Study subjects were not required to wear masks at home. Their family members/visitors were neither taxed to wear masks in public nor were they tested for asymptomatic Covid, which is often spread in homes (2). Accordingly, it is plausible, if not likely, that some study subjects caught Covid in their own homes. This critical design flaw prevents any conclusion about the efficacy of masks for preventing Covid; a nuance that will be lost on non-scientists. Nonetheless, the erroneous conclusion was immediately trumpeted, using the imprimatur of Annals, to challenge mask-wearing. The effect – albeit inadvertent – is almost certain to be greater morbidity and mortality.
Regarding "Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers"
We commend the authors of the study on broaching a much-debated subject in the current environment. The trial was designed to obtain the most power to detect a difference. Unfortunately, there were confounding variables that were unaccounted for and unmeasured.
There is a flaw in primary outcome ascertainment. False-negative rate and false positive rate of antibody testing, PCR, and diagnosis all vary widely. For example, sensitivity (IgM and IgG) of the antibody kit in this study (86.7% and 66.7%, respectively) is equivalent to a 64.6% PPV with a 5.0% prevalence [1]. This is even more pertinent in the low prevalence (1.2%) Danish population [2], [3].
Individuals who could not correctly perform the test were assumed negative, which would further skew the data. Additionally, the intention group attrition was higher than the control group (638 vs. 524). The characteristics of the study participants’ households would heavily affect the data set as well. If family or house members were COVID-19 positive, mask-wearing outside of their homes would not protect them from their highest risk source (their homes).
We contest that an intent-to-treat analysis is inappropriate, given the authors’ own published intervention adherence rate (46%). Multiple imputation analysis is simply an amplification of the data set and agreement between the original data set is a moot point. The homogeneous Danish population would make it difficult to externally validate this to other much more heterogeneous populations (i.e. New York).
It is questionable if the study is a true RCT as it lacked blinding and utilized a self-reported and self-measured primary outcome which opens it up to a majority of biases. Although the researchers cited their study for the equivalence of self-testing with healthcare professional testing, this may be inappropriate for research purposes and better suited for pandemic infection control [5].
Although the goal of the study was to publish the researchers’ heard-earned data, contextualization in these volatile times is paramount. This study received 90,000 tweets by 60,000 users within 4 days of publication [4]. The majority of these tweets championed the study as evidence of the impotence of masks in the control of the COVID-19 pandemic. The authors of the study would agree that this is a gross misinterpretation of the research, which further points to the fact that the wording of the conclusion should have been chosen slightly more judiciously.
References:
[1] Serology Test Evaluation Report for “Livzon IgM/IgG Diagnostic Kit for IgM/IgG Antibody to Coronovirus (SARS-Cov-2) Lateral Flow” from Zhuhai Livzon Diagnostics Inc. Food and Drug Administration website. Updated June 10, 2020. Accessed November 22, 2020 https://www.accessdata.fda.gov/cdrh_docs/presentations/maf/maf3285-a001.pdf
[2] COVID-19 surveillance. Current data on the development of coronavirus/COVID-19. Danish Health Authority website. Updated November 20, 2020. Accessed November 22, 2020.https://www.sst.dk/en/english/corona-eng/status-of-the-epidemic/covid-19-updates- statistics-and-charts
[3] Denmark Population (Live). Worldometer website. Updated, November, 22, 2020. Accessed November 22, 2020. https://www.worldometers.info/world-population/denmark-population/
[4] Article metrics. Annals of Internal Medicine website. Updated November 22, 2020. Accessed November 22, 2020. https://annals.altmetric.com/details/94531651/twitter
[5] McCulloch DJ, Kim AE, Wilcox NC, et al. Comparison of Unsupervised Home Self-collected Midnasal Swabs With Clinician-Collected Nasopharyngeal Swabs for Detection of SARS-CoV-2 Infection. JAMA Netw Open. 2020;3(7):e2016382. doi:10.1001/jamanetworkopen.2020.16382
Disclosures:
No disclosure to claim.
Thought experiments and science predict that facemasks reduce viral loads and reduce severity of infection
The study is misleading; it did not consider adequately too many critical variables (factors) that have major impact on measured outcomes. Thought experiments from science predict that facemasks reduce viral loads and severity of infection.
Statistics describe outcomes, but does not explain causes. It is impossible to conduct experiments on all possible observations and outcomes, and it is not necessary. We can use “thought experiments”, which Einstein used to create Relativity. We had data on the movement of planets for over 100 years, but it took “thought” experiments for Newton to predict planetary movement via equations.
We understand enough about viruses to know the body produces and expels them, mostly via mouth and nose. We know an infected person can expel many viruses. A well-designed mask, and substantial obstruction, will reduce the number of virus expelled far into the air. A mask will absorb viruses. This is not “genius” physics. I knew about it since I was about 6 yo. My parents taught me to use a handkerchief, hold it to my nose, to prevent spreading “stuff” when I cough. It worked. There is no doubt that holding a paper towel or similar paper or cloth to the mouth reduces the amount of “stuff” going out when I cough.
To those who doubt it and need more “studies”, I propose they put themselves in front of people coughing without covering their mouth. Although it may not infect them, the fluids they get in the face and mouth will provide evidence of how facemasks work.
Thus, a thought experiment and science provide probative evidence that facemasks can reduce the amount of “stuff” an infected person sends to the air. How much of a reduction depends on the nature of the facemask, how tight it is, how much it absorbs and retains fluid, etc. If everybody used facemasks in public places, viral loads in public places are reduced.
We do not need more studies of the obvious; we do not need a sample size of 1,000 people thrown out of 10th story windows to predict broken bones when they hit the concrete sidewalk. If a study of 10,000 people who took Vitamin EZY434 proved they fly like birds, I would not believe it because my thought experiment says it cannot be true.
Similarly, facemasks reduce particles absorbed from air. Known for years in construction, surgery, labs, etc.
Cluster randomization and adherence assessment are needed to test masks’ true potential
We read with interest the study evaluating mask mandates in Denmark by Bundgaard and colleagues.1 We commend the authors for performing a randomized trial of a non-pharmaceutical intervention in the midst of the pandemic. However, the study makes it difficult to draw conclusions about the impact of masks in preventing incident infection or severe COVID-19. Although masks were provided and recommended to participants, masking was not commonplace in Denmark at the time, and 14% of participants reported experiencing social harms due to masking. Only 46% of participants reported wearing a mask as recommended, and overreporting of adherence, as has been seen in previous prevention studies for stigmatizing interventions,2 likely occurred. Notably, due to the complexity of interpreting self-reported adherence, HIV and sexually-transmitted infection prevention trials are now designed to incorporate objective assessment of adherence.
The study would have benefitted from inclusion of implementation science principles: understanding the desired behavior in its social context, cluster randomization, and assessment of intervention fidelity.3 Recommending a potentially stigmatizing intervention in a minority of individuals within a community is, we believe, a major flaw in a study designed to evaluate a policy intervention. Cluster randomization would have allowed an entire community to be randomized to the recommendation, minimizing social harms to the individual and likely increasing intervention adherence. Assessment of intervention fidelity and acceptability, such as through direct observation within the community, would allow a more accurate interpretation of self-reported adherence data.
Use of cluster-randomization has other benefits. Masks are likely to be more effective in preventing forward transmission, in the context of high community uptake and adherence. By randomizing isolated members in the community to the mask recommendation, this study design cannot answer if “masks protect you.”4 Second, given the high proportion of asymptomatic COVID-19 infections, we do not know how many individuals were infected within their household bubbles. An optimal design would pursue a cluster-randomized approach, with sufficient power to detect incident (with PCR) rather than prevalent (with serology) infections, and assess disease severity via cataloging clinical outcomes (do masks lead to less severe infections via reduced inoculum?5). A mask recommendation for isolated members of a community is unlikely to be effective. We suggest that future studies assess the impact of recommendations to wear masks at the community-level, which will be more informative for public health officials trying to stem transmission and disease while awaiting an effective and widely available vaccine.
Authors state major limitations of study
The authors state the limitations of the study: Inconclusive results, missing data, variable adherence, patient-reported findings on home tests, no blinding, and no assessment of whether masks could decrease disease transmission from mask wearers to others. Asian countries have very low levels of COVID and for decades people wear mask if they think they have flu or a cold. The authors clearly state they could not assess this.
This is extremely inadequate research to support forcing the entire world to wear masks
Before making any recomendations to wear masks adequate research would be needed but this hasn't occured. Whilst such measures are often described as a recommendation in the real world people are being forced to wear masks and in some countries quite agressively. This study finds no significant effects in relation to the alleged Sars-cov2 but does not look at the many other possible effects of wearing these. For example there has been a doubling in shootings in NY this year. Could the masks be contributing to this? What are the effects on overall health? What are the dangers of conditioning people to accept forced medication in violation of informed consent laws? Without having done any proper research to establish the long term effects it is incredibly reckless to be forcing masks on the entire world and this study shows how little is known about it. It is time to immediately end these impositions and any further experimentation on the public.
This study design would not even proof that a 100% protection has a protective effect
Imagine a 100% perfect protection against COVID-19 (a hermetic room), what outcome should be expected for this by-definition safe group using this study design?
Here is the math only for estimating
- the false-positive antibody-tests
- positive test due to before-baseline infections
But as the study design grants protection at average only 4.5 hours/day further infections outside the room (in the study false-classified as noneffective protection) should be added to the calculated expectations.
The study reports antibody testing has an estimated 99,2% specificity. For about 2400 tests this leads to an expectation of 2400*0.008=19 false-positive tests in each antibody test group.
IgG-antibodies form very delayed and persist very long. So in non-increasing rate of new infections (as the case in 05/2020 in Denmark) about 80% of all true-positive IgG tests at study-end show infections before study-baseline. So the expectation of positive tests due to before-baseline infections in the control group is 10.4 (80% of 13 (=32-19) „true-positive“ IgG tests)
The mentioned false-detection arises solely by a test-property (specificity) and before-baseline events, so the expectations for the control group for false-positive test (19) and for true-positive tests due to before-baseline infections (10.4) equals the expectations for the safe group, adding up to: expectation(IgG-SafeGroup)=29.4
IgM-tests respond from >2-6 weeks after infection. So about 50% of the IgM true positive tests are likely due to before-baseline infections. Analogue to above 19 false positive and 9 positive IgM tests (50% of 18 (=37-19) „true-positive“ IgM tests) due to before-baseline infections sum up to: expectation(IgM-SafeGroup)=29
PCR-tests hardly suffer from specifity and time lags in the study, so no positive PCR-tests should be expected in the safe group: expectation(PCR-SafeGroup)=0
A temporally evenly distributed health care diagnosis during study will again suffer from the delay from infection to diagnosis (first 9 days (=30% of 30 days) diagnosis will likely show before-baseline infections). So 0,3*10=3 cases are likely due to before-baseline infections and have to be expected for the safe group as well: expectation(HealthCare-SafeGroup)=3
Even without additional expected infections at home, friends etc. - falsely assigned as inside the hermetic room the expected outcome in the by-definition safe group is already about 75% of the control outcome (or 90% of the face-mask-group).
Altogether this study design expects for a by-definition 100%-protection:
- measure an Odd Ratio of ≥0.75 (≤25% protection),
- include OR=1 (i.e. no-protection-at-all) in the 95%-Confidence Interval and
- exclude OR≤0.4 (≥60% protection) from 95%-CI
Mis-leading study . Results need to be made more clear.*” Exposure was to persons NOT wearing masks”*
This study does NOT show that mask wearing in ineffective in mitigating the spread of Corona Virus / COVID-19 / SARS-CoV-2. It shows (what we already knew) that wearing a mask does not protect the person wearing the mask as much as we would like. The reason you wear a mask is to keep your viral particles to yourself - don't spread them to others. Unfortunately, anti-maskers are using this study as "prof" that they don't need to wear masks. This is irresponsible and should be made clear in the title of the study. From the discussion: "The findings, however, should not be used to conclude that a recommendation for everyone to wear masks in the community would not be effective in reducing SARS-CoV-2 infections, because the trial did not test the role of masks in source control of SARS-CoV-2 infection. During the study period, authorities did not recommend face mask use outside hospital settings and mask use was rare in community settings (22). This means that study participants' exposure was overwhelmingly to persons not wearing masks."
Will mandatory mask usage be scaled back in light of these results?
Dr Bundgaard and colleagues are to be congratulated on this well-constructed randomised trial, at a time when much policy has been based on weak observational or laboratory-based studies. Their results highlight the dilemma that lack of evidence for benefit is unlikely to alter public policy. The suggestion that mask wearing is for the protection of others, rather than of the wearer, has created a climate of discrimination against those with genuine medical exemptions. This is especially worrying when applied to school children, known to play a very small role in transmission of Sars-Cov-2. In particular, the creeping use of masks in classrrooms in the UK, has resulted in many reports of children feeling alienated and unable to understand their teachers. Parents of primary school children are being instructed to wear masks when collecting their children from the school playground, giving children a potent message that they and their parents are all a danger to one another. The long-term mental health impacts of this are yet to be fully realised.
Mis-representation of research purpose
Members of the general public are referencing this research as a battle cry that communities do not need to wear masks in public. After reading the entire article, I ascertained that telling the general public to stop wearing masks was not the purpose or outcome of this research.
During these tumultuous times it might be a moral imperative to include some type of explanation with this research. Very few individuals outside of the medical profession will take the time to thoroughly read the article and analyze the outcomes.
Sincerely,
Brenda Marfin, Ph.D.
Unassociated at this time while caring for my husband with end stage renal disease and Alzheimer's. I depend on the kindness (and myself) of others to wear a mask.
In absence of an objective mechanism to track the intervention what are we counting?
The effort by Dr. Bundgaard and colleagues is commendable. However, the trial design and the associated results remind me of the randomized controlled trials assessing the efficacy of a "prayer" intervention. The fundamental issue with mask intervention and social distancing, like prayer, is the lack of objective mechanisms to ensure and track compliance or non-compliance (lack of an accurate method to track who is praying or not praying). As an example, the authors state that only "46% of participants wore the mask as recommended" in the mask group but failed to ask participants in the no mask group about their usage of the mask. Furthermore, a mask is considered an added layer of protection with social distancing and therefore the mask's added effects would be challenging to deduce. Accordingly, given this basic challenge of delivering an intervention without tracking/confirmation mechanism, the results, at best, can be considered anecdotal. The desire for evidence from a randomized controlled trial for an intervention question is understandable. However, logistical challenges associated with the reliable implementation of the intervention (i.e., mask) and tracking of adherence makes the conduct of a randomized trial to assess the efficacy of mask a non-starter. The efficacy of a mask needs to be framed in the context of reducing the risk and not binary choices of works or does not work.
Please *clarify* your policy recommendations
In light of your recent research, will you please clarify your policy recommendations? Thank-you
Tested recommendation, not adherence to recommendation
While I commend the researchers and it does demonstrate whether recommending masks provides benefit, the experiment does not demonstrate whether mask-wearing actually took place. Research in other arenas has shown people are not honest when providing answers to surveys, and these people would have likely had reason to be less than honest about the frequency with which they wore a mask and the coverage of their mouth and nose while wearing one. It may be better to find people with serious concern about NOT wearing a mask to act as the experimental group, and those who are entirely opposed to mask-wearing as the control group. This would be answer the question of whether wearing a mask provides benefit. I think people are misunderstanding the intent of this study, which was to test the power of recommendation with the hope that those in the experimental group would be honest in their responses. We will never know if they were honest or used the masks properly.
Risk for bias?
An important large-scale study investigating the benefit of bearing a mask to reduce the risk of aquiring COVID-19 during an daily average of 4,5 hours stay outside the home during one month.
To be able to do that, one must eliminate the possible bias that the participants are instead infected during the daily 19,5 hours they stay at home.
A total of 52 participants in the mask group and 39 control participants reported COVID-19 in their household. Of these, 2 participants in the face mask group and 1 in the control group developed SARS-CoV-2 infection…'
However, more participants may have been exposed and infected by household members, without participants reporting COVID-19 in their household, if the members experienced asymptomatic infection or only mild disease, not suspected to be due to COVID-19.
The possible inclusion of misdiagnosed subjects - infected trough household contact but estimated as infected during outside the home should influence both groups - with or without masks - equally. And the true difference between the groups, and thus the benefit of wearing a mask, should increase if this bias had been controlled, although with wide confidence intervals, due to the relatively low number of infection.
The reported finding of only 3% (3/95) infected through household contacts during the study appear to be surprisingly low, supporting the proposed risk for bias, due to misdiagnosis.
Perceptual error in viewing COVID-19 spread as linear, not exponential.
In the discussion section the authors state that "Testing at the end of follow-up, however, may not have captured any infections contracted during the last part of the study period, but this would have been true in both the mask and control groups and was not expected to influence the overall findings.". This statement assumes a linear spread of infection among both groups. COVID-19 however has been spread exponentially (Lammers, Crusuis, Gast 2020). As such infections contracted during the last part of the study period would be largely significant to the overall findings.
Timing is everything
This study pooled participants from two cohorts split two weeks apart in the months following the peak of first wave of infections in Denmark.
Self-reported pre-study baseline seropositive prevalence was 1.7% and these participants were excluded from the study.
Of those with unknown baseline seropositivity, 2% were positive at the end of the study.
Of those with known baseline seropositivity, around 1.7% appear to have seroconverted during the month of the study.
Do these very similar percentages spread across time raise concerns about the false positive rate of the self-reported antibody test used in a low prevalence population?
Even without false positive rate, to achieve 80% sensitivity, this lateral flow antibody test has to be performed at least 15 days after symptom onset. It takes an average of 5-6 days to develop symptoms following exposure, so this creates at least a 3 week lag. Given the study only lasted 1 month in each cohort, any protective effect of mask-wearing will be diluted by late sero-conversions infected prior to the study. This effect will be balanced in the control group, but still increases the OR towards 1 even if masks were having an effect when both groups are pre-loaded equally. Taking this into account and any post-study seroconversions missed in the control group could possibly have led to a significant result. The PCR and clinically diagnosed outcomes will not suffer from this lag so much, and it is noteworthy that mask wearers scored 0 and 5 cases respectively versus 5 and 10 for controls, whilst IgG seropositivity was higher than IgM in mask wearers and vice versa in controls.
The study was also underpowered for detecting a protective-to-wearer effect of somewhere less than 50% which could be a more reasonable estimate of efficacy.